A Soap Notes Counseling Template is a structured document that allows mental health professionals to record detailed notes about their sessions with clients. It provides a standardized format for documenting essential information, ensuring consistency and facilitating communication among healthcare providers. A well-designed template is crucial for maintaining accurate records, adhering to ethical guidelines, and providing effective treatment.
Key Components of a Soap Notes Counseling Template
1. Client Information: This section should include the client’s name, date of birth, contact information, and insurance details.
2. Date and Time of Session: Clearly indicate the date and time the session took place.
3. Presenting Problem: Briefly summarize the client’s primary concerns or presenting issues.
4. Goals: Outline the specific goals the client and therapist have set for the session or treatment plan.
5. Assessment: Document the therapist’s observations and assessment of the client’s mental state, including mood, affect, thought processes, and behavior.
6. Interventions: Describe the therapeutic techniques or interventions used during the session, such as cognitive-behavioral therapy, psychodynamic therapy, or supportive counseling.
7. Plan: Summarize the plan for the next session or treatment plan, including any referrals or follow-up appointments.
8. Signature: The therapist’s signature and credentials should be included at the bottom of the template.
Design Elements for Professionalism and Trust
1. Clarity and Organization: A well-organized template is easy to read and understand. Use clear headings, bullet points, or numbered lists to separate different sections.
2. Consistency: Maintain consistent formatting throughout the template, using the same font, font size, and spacing. This creates a professional and polished appearance.
3. Professional Language: Use clear and concise language that is appropriate for a professional setting. Avoid jargon or overly technical terms that may be unfamiliar to others.
4. Confidentiality: Ensure that the template protects the client’s privacy by avoiding the use of personally identifiable information in the document title or file name.
5. Legal Compliance: Adhere to any legal or ethical requirements for documenting mental health sessions. This may include specific guidelines for record retention or consent procedures.
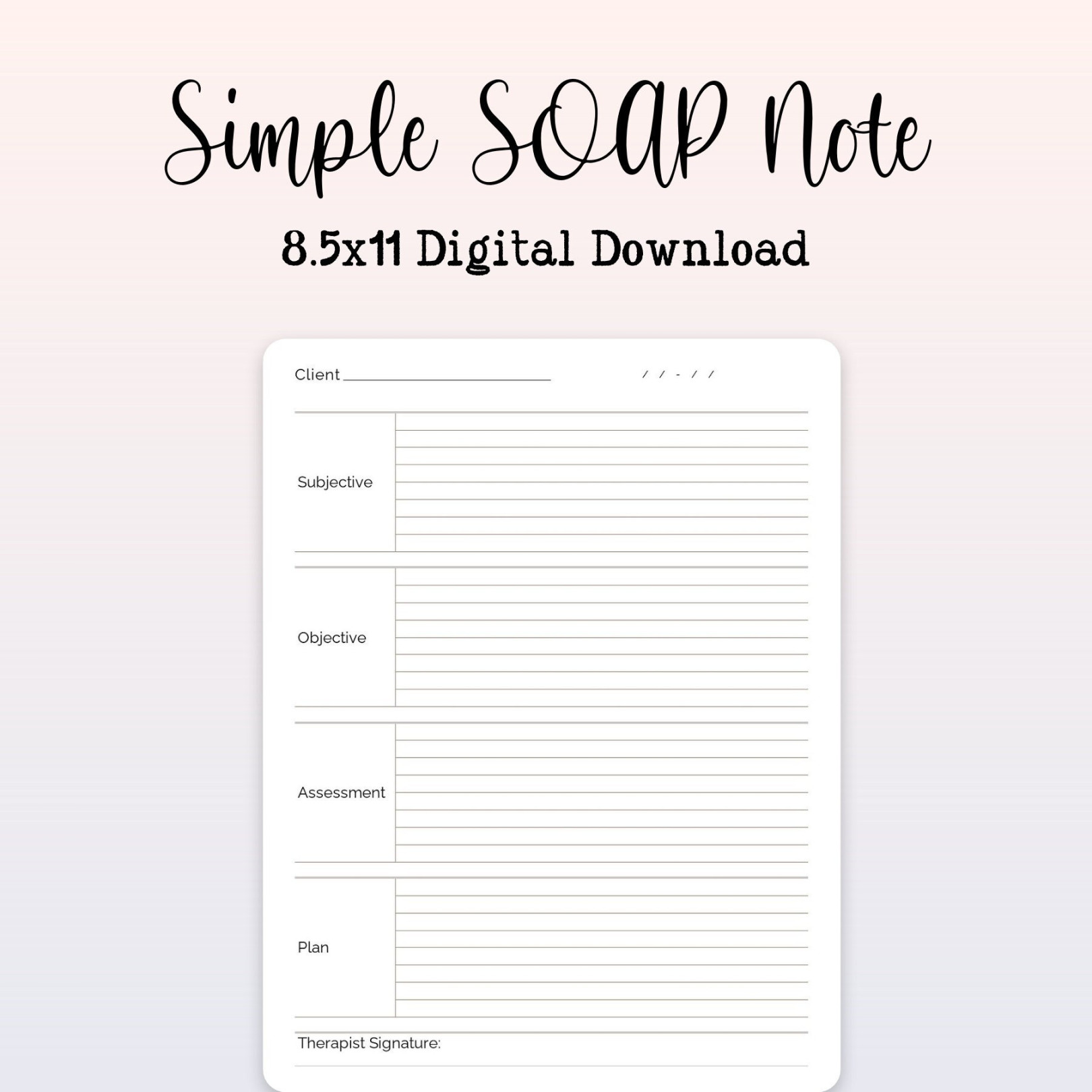
Example Template Structure
Client Information
Name:
Session Details
Date:
Presenting Problem
Goals
Assessment
Mental State:
Interventions
Plan
Signature
Therapist’s Name:
Additional Considerations
Electronic Templates: Consider using electronic templates to streamline the documentation process and improve efficiency.
By following these guidelines and incorporating the recommended design elements, you can create a professional Soap Notes Counseling Template that effectively documents your sessions and fosters trust with your clients.